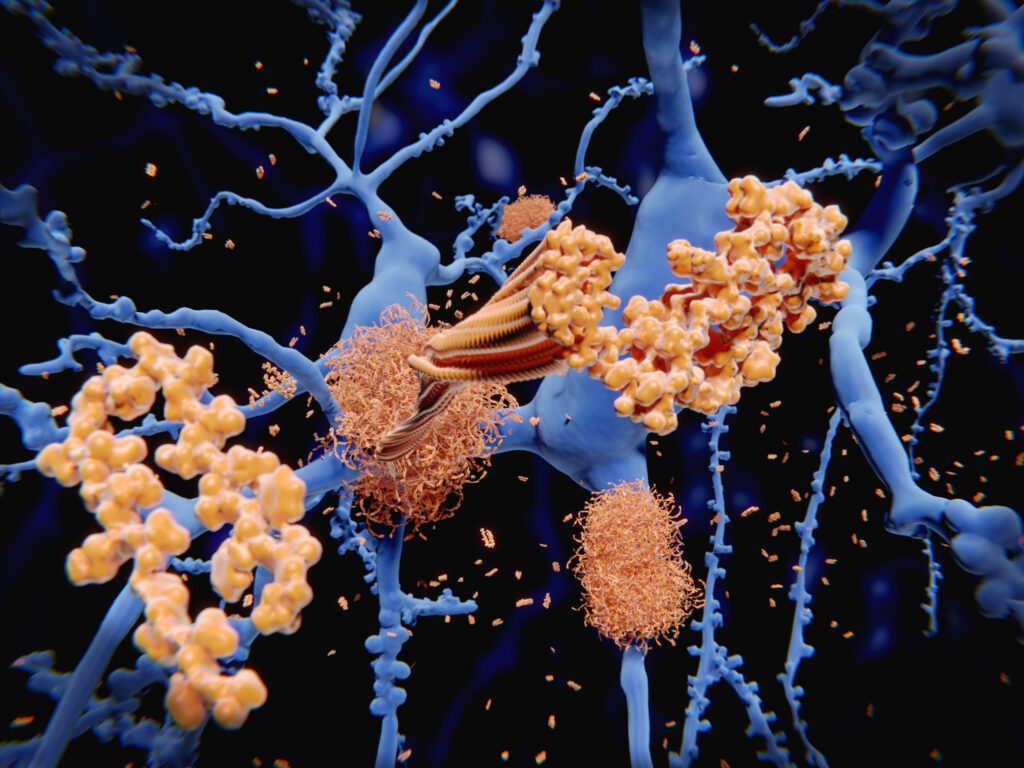
Researchers at the University of Strathclyde, Scotland, and the Italian Institute of Technology have developed a fiber-optic technique to detect amyloid plaques in the brains of freely moving mice. The new technique, published in Neurophotonics, uses the fluorescent dye Methoxy-X04, which binds specifically to amyloid fibrils and can cross the blood-brain barrier, allows researchers to track the presence and distribution of plaques in the brains of mouse models of Alzheimer’s disease.
The team’s findings demonstrated that fiber photometry, which today is typically used to measure neural activity, can be adapted to detect molecular pathology in Alzheimer’s mouse models. Their approach could potentially eliminate the need for genetically encoded sensors and would allow for longitudinal measurements of amyloid in the same mouse model. Current methods to measure amyloid accumulation in mouse models requires examination of post mortem brains.
“This means that scientists can now test how potential treatments affect plaque buildup in real time, accelerating the development of new Alzheimer’s therapies,” the researchers wrote in a press release stated.
The new method was developed in two phases. First, the researchers used conventional flat optical fibers to detect fluorescence signals in anesthetized mice after injecting Methoxy-X04. In this phase, the researchers showed that the depth profile of the in vivo signals closely correlated with post-mortem histological data. Using machine learning algorithms the team was also able to differentiate between mice with Alzheimer’s and healthy animals based on these profiles.
Second, they introduced tapered optical fibers (TFs), which can capture light from multiple depths. These fibers were implanted into the brains of living mice and allowed the researchers to monitor depth-specific plaque accumulation in awake, freely moving animals. Their data showed that the fluorescence signal increased with age in the Alzheimer’s model mice, consistent with disease progression.
“Our approach expands the capabilities of fiber photometry to monitor molecular pathologies, such as amyloid plaques, even in a freely behaving condition,” the researchers wrote.
This new method has promise to address a longstanding challenge in preclinical Alzheimer’s research, namely the reliance on post-mortem tissue analysis, which makes it impossible to monitor dynamic changes in plaque development or therapeutic response over time in the same mouse. Other imaging techniques like two-photon microscopy and optoacoustic tomography can be used for in vivo imagining of plaques, but have limited utility.
“Although optoacoustic tomography allows monitoring of brain-wide plaque signals, the imaging needs to be done under anesthesia,” the researchers wrote in the discussion. “Our approach offers a unique, novel solution to monitor depth-resolved plaque signals in a freely behaving condition.”
The development of this technique builds on earlier research that showed the feasibility of using Methoxy-X04 as an imaging agent for plaques through other optical methods. There are limitations to this technique, however. Methoxy-X04 requires excitation at approximately 405 nm, but requires a dedicated laser system, which is not found in many testing labs.
Also, while the method can determine the total level of plaque within the brain, it does not have the ability to identify individual plaques, such as amyloid-β, the plaque that drives progression of AD.
Despite these shortcomings, the researchers said their results demonstrate that the depth-resolved fiber photometry approach can be adapted for detecting extracellular pathological features, which expands its application beyond neuronal activity tracking.
The team will now look to optimize the taper geometry of this technique to improve spatial resolution, integrate additional light wavelengths for combined functional and structural imaging, and test the method in conjunction with therapeutic interventions.
Their new fiber-optic method “opens a new avenue for preclinical applications of TF-based technology in neurodegenerative disease mouse models,” the researchers wrote.