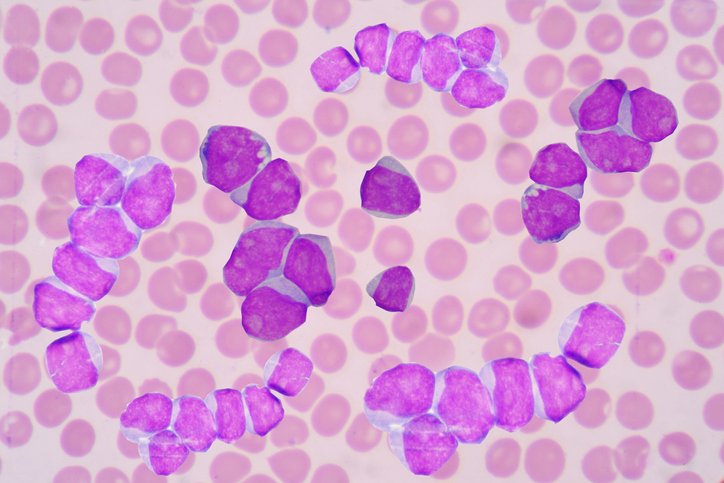
Despite major advances in immunotherapy—including the 2025 Nobel Prize in Physiology or Medicine recognizing advances in peripheral immune tolerance—progress against leukemia has remained limited. Acute myeloid leukemia (AML) continues to defy immune-based treatments, reflecting an incomplete understanding of how leukemia cells evade the immune system.
Lund University researchers have now uncovered one of these evasive tricks and have shown how to disable it. In a study titled “Aberrant expression of SLAMF6 constitutes a targetable immune escape mechanism in acute myeloid leukemia,” published in Nature Cancer, the team identified a surface protein, SLAMF6, that acts as an immune-suppressive shield on AML cells. By engineering an antibody to block SLAMF6, the researchers restored T cell activity both in vitro and in humanized mice, reactivating the immune system’s ability to kill leukemia cells.
“We wanted to see if we could find surface proteins unique to leukemia stem cells, and which would therefore act as interesting targets for a targeted treatment,” said Thoas Fioretos, MD, PhD, professor of clinical genetics at Lund University and senior consultant at Skåne University Hospital. “If such proteins were not present on healthy blood stem cells, it might be possible to attack the tumor—without harming the healthy blood system.”
To pinpoint AML-specific antigens, the researchers began with a large-scale screen of 362 cell-surface markers in leukemia-enriched samples, comparing them with healthy bone marrow. SLAMF6 emerged as a clear outlier—present in roughly 60% of AML cases, but absent on normal hematopoietic stem and progenitor cells (HPSCs). Using single-cell RNA sequencing, they confirmed that SLAMF6 expression was restricted to malignant cells and a few immune lineages.
The authors reported that mouse to human translation is complicated by the varying expression patterns of SLAMF6, writing, “… the expression in humans is limited to T cells, B cells, NK cells, and eosinophils, murine SLAMF6 is also expressed on neutrophils and all HSPC populations. SLAMF6 knockout would, thus, be expected to induce distinct phenotypes in humans and in mice, emphasizing the importance of further studies in human and humanized models.”
Functional studies using CRISPR/Cas9 gene editing revealed that knocking out SLAMF6 in AML cell lines released the brakes on T cells. Without the protein, T cells became activated and destroyed leukemia cells in co-culture experiments. “When we blocked the surface protein, using a specific antibody we developed in cooperation with the SciLifeLab Drug Discovery and Development Platform, the T cells could suddenly detect and kill the cancer cells—both in test tubes and in mice,” said co-corresponding author Carl Sandén, PhD, a researcher at Lund University. The human SLAMF6 antibody, called TNC-1, “…binds the homodimerization interface with high affinity and disrupts the SLAMF6–SLAMF6 interaction,” the authors wrote.
“Our discovery can partially explain why immunotherapies have thus far only had a limited effect in AML. It’s an important step forward, but continued research and clinical trials will be needed before it can be relevant as a treatment for a patient group that is in great need of new therapies,” added Niklas Landberg, MD, PhD, research group leader at Lund University and medical registrar in hematology at Skåne University Hospital.
They wrote, “In conclusion, we show that aberrant expression of SLAMF6 is a common and targetable immune escape mechanism that could pave the way for immunotherapy in AML.” The researchers have launched Lead Biologics, a spin-off to advance the SLAMF6-blocking antibody toward clinical testing. Next steps include further preclinical validation and safety studies aimed at translating the discovery into clinical trials.