For years, scientists have tried to harness bacteria’s ability to infiltrate tumors, but safety and control have remained obstacles. Now, a study published in Oncotarget demonstrates that an engineered strain of Salmonella Typhimurium, called ACTM-838, can safely deliver immune-activating payloads directly to solid tumors and trigger a durable anti-tumor response.
The work, led by Kyle R. Cron, PhD, and Akshata R. Udyavar, PhD, at Actym Therapeutics, builds on decades of research in bacterial immunotherapy but pushes it into a new era of precision design.
“ACTM-838 showed durable anti-tumor efficacy in multiple murine models and synergized strongly with anti-PD1 therapy,” the authors write.
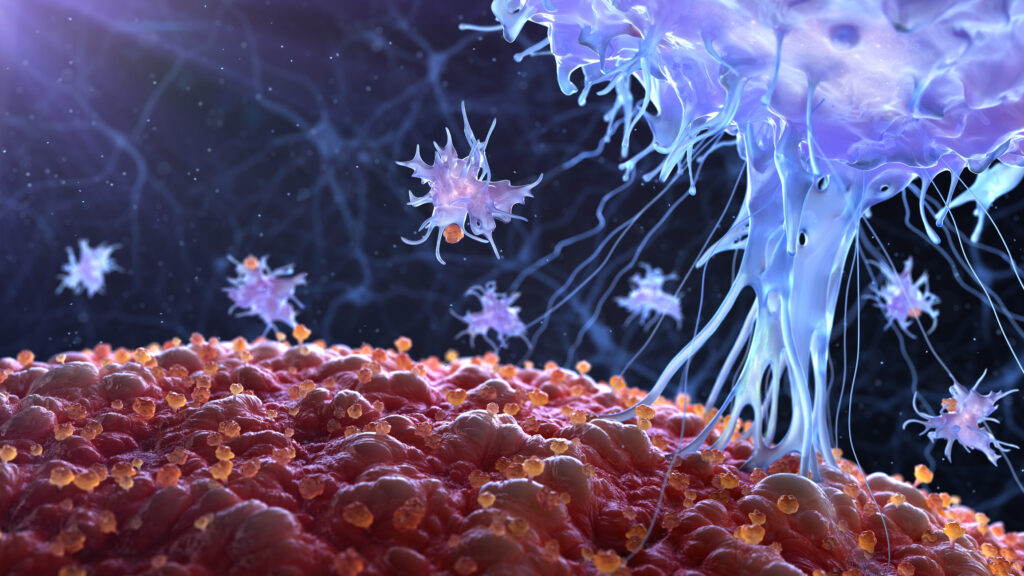
Turning tumors from immune-cold to immune-hot
Solid tumors often suppress immune activity within their microenvironment, making it difficult for checkpoint inhibitors to work. ACTM-838 was designed to overcome this by targeting phagocytic immune cells in the tumor microenvironment (TME) and delivering two key immune-stimulating payloads:
- IL-15/IL-15Rα, a cytokine complex that drives expansion of natural killer (NK) and cytotoxic T cells, and
- a cyclic-di-AMP STING agonist, which activates innate immune pathways and type-I interferon signaling.
Together, these payloads promote a shift from an immunosuppressive to an immunostimulatory TME—effectively “reprogramming” the tumor’s local ecosystem.
The study describes ACTM-838 as part of the company’s broader STACT platform (Systemic Targeted Activation of Cell Therapy), a modular, live-attenuated bacterial system that allows multiplexed delivery of genetic payloads after intravenous injection.
Precision targeting, reduced toxicity
Historically, bacterial therapies have been limited by systemic inflammation and poor control over where the microbes localize. The Actym team overcame these issues through genetic attenuation and optimization of tumor-specific enrichment, ensuring the bacteria thrive in the oxygen-poor, nutrient-dense tumor environment while sparing healthy tissue.
In animal studies, ACTM-838 accumulated almost exclusively in tumors within 24 hours of administration, while bacterial counts in healthy organs dropped rapidly—demonstrating on-target selectivity and improved tolerability compared to earlier bacterial constructs.
Broad and lasting anti-tumor immunity
In preclinical mouse models—including EMT6 breast, CT26 colon, and B16-F10 melanoma tumors—systemic administration of ACTM-838 produced marked tumor regression and, in some cases, complete responses. Mice cured of their tumors resisted subsequent tumor rechallenge, indicating long-term immune memory.
When combined with anti-PD1 checkpoint inhibitors, the therapy achieved even greater control of tumor growth, suggesting that it may unlock the full potential of checkpoint blockade in previously refractory settings.
At the cellular level, single-cell RNA sequencing revealed a profound remodeling of the tumor’s immune composition. The treatment increased cytotoxic CD8⁺ T cells, proliferating macrophages, and antigen-presenting dendritic cells, while reducing M2-like tumor-associated macrophages (TAMs) and regulatory T cells (Tregs).
Differential gene expression analyses confirmed upregulation of interferon-stimulated genes, antigen presentation machinery, and glycolytic metabolism, all consistent with a reinvigorated immune microenvironment.
A bridge between innate and adaptive immunity
By co-delivering IL-15 and a STING agonist, ACTM-838 engages both innate and adaptive immune arms—a dual activation rarely achieved by traditional immunotherapies. “This synergy allows the immune system to mount a coordinated, durable response rather than a transient one,” the authors note.
Importantly, systemic inflammation and cytokine release were markedly reduced compared to earlier bacterial therapies, underscoring the platform’s translational promise.
Actym Therapeutics has initiated a Phase I clinical trial of ACTM-838 in patients with advanced solid tumors (NCT identifier pending). The company envisions its bacterial platform as a modular delivery vehicle for a range of immunostimulatory payloads beyond IL-15 and STING, adaptable for combination regimens or tumor-specific customization.