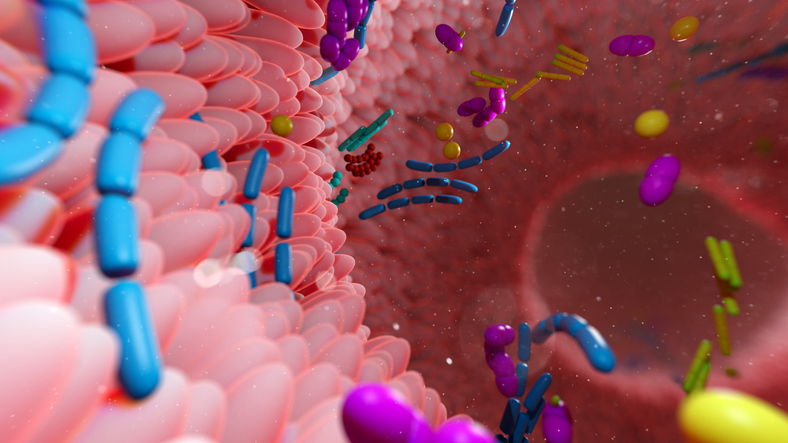
A UCLA-led research team has identified a genetic system in gut bacteria that helps them adapt rapidly to the human gut microbiome, a finding that could change the current understanding of this vital component of human health and suggest new ways to enhance it as a method to treat a variety of diseases. The study, published in the journal Science, focused on how diversity-generating retroelements (DGRs), which carry collections of genes that work together to create random mutations in specific hotspots in bacterial genomes, accelerate bacterial evolution and allow the microbes to change and adapt.
“One of the real mysteries in the microbiome is exactly how bacteria colonize us,” said senior author Jeff F. Miller, PhD, director of the California NanoSystems Institute (CNSI) at UCLA, and a professor of microbiology, immunology, and molecular genetics. “It’s a highly dynamic system intimately connected with human physiology, and this knowledge about DGRs could one day be applied for engineering beneficial microbiomes that promote good health.”
DGRs were first discovered in the Miller lab at UCLA and are more abundant in the gut microbiome than in any other known environment. But despite their prevalence, the functional role DGRs in the gut has remained largely unstudied.
To study how DGRs function in the gut, the team focused their work on Bacteroides, a dominant genus in the human microbiome. Analyzing 618 isolates from 29 Bacteroides taxa, the team identified more than 1,100 distinct DGRs. From this population, the researchers were able to group the DGRs into 35 protein families across three broad categories: pilins and pilin-like proteins, cytoplasmic kinases, and viral receptor–binding proteins.
Drilling down, the UCLA team narrowed their focus to the DGRs that diversify pilin proteins, the elements that form pili, hairlike features that help bacteria attach to surfaces or one to each other. They found that many DGRs targeted binding domains at the very tips of the pili that allowed the bacteria to “fine tune” what they would adhere to in different environments.
“We think DGRs allow the bacteria to rapidly change what their pili can adhere to,” said first author Ben Macadangdang, MD, a neonatologist at UCLA Health. “A bacterium may be optimized for one person’s gut, but if it goes out and tries to colonize someone else, it encounters a very different environment. Finding something new to bind to gives the bacteria an advantage, and we think that’s why we see so many DGRs within the microbiome.”
The team also discovered that DGRs are not confined to individual bacteria strains. Through a process called horizontal gene transfer, DGRs can move between bacteria, spreading this adaptive potential across microbial communities.
To test how DGRs function under real-world conditions, the team used in vitro systems and germ-free (gnotobiotic) mice. In monocolonized mice, DGRs produced random protein variants. But in competitive microbial environments, DGR-modified proteins generated similar structures despite genetic differences, providing evidence of positive selection and adaptive pressure.
The team also extended their research to analyze large-scale metagenomic data from mother-infant pairs. These data showed that specific DGRs were inherited from mothers and became active in infants, generating new protein variants that supported microbial colonization.
“The developing microbiome is connected to our developing immune system, and that primes us for the rest of our lives,” Macadangdang said. “When the microbiome is disrupted, we see higher rates of chronic disease later in life. This presents a strong opportunity to engineer the infant gut microbiome to prevent these risks.”
The researchers wrote, “This study reveals that DGRs are widespread, dynamically regulated, and functionally consequential components of the gut microbiome. By enabling targeted hypervariability in proteins involved in adhesion, signaling, and other functions, DGRs are poised to contribute to microbial adaptability during ecological transitions and competitive interactions.”
With changes in the microbiome linked to diseases such as Crohn’s disease, metabolic syndrome, and colon cancer, the new findings provide a fertile ground for exploring and developing future microbiome-targeted therapeutics.
Next steps for the researchers include additional use of lab-based models and further observational studies in human populations. The team hopes to find out how to manipulate DGRs in ways that either encourage proliferation of beneficial microbial strains or suppress harmful ones, particularly during early-life development.
“We’re at this really early stage,” Miller said. “There are so many questions that this raises, we’re just realizing how much we don’t know about DGRs in the microbiome, or what exploiting them for applications could yield. I’ve never been more excited about what’s going to come next.”