Genetically editing a single nucleotide base could clinically correct cardiomyopathies, preclinical research suggests.
The study, in the Proceedings of the National Academy of Sciences, demonstrates the power of base editors to correct disease-causing point mutations, where a solitary change in the DNA sequence can have devastating consequences.
Using the well-established CRISPR/Cas system, the base editing process enables single nucleotide changes without introducing double-strand DNA breaks.
In the current research, it was able to correct cardiac disease caused by mutations in Lamin A (LMNA) gene, which codes for membrane proteins separating the nucleus and the rest of a cell.
“Our work represents an important step toward the potential clinical correction of cardiomyopathies using gene editing tools,” asserted Xurde Caravia, PhD, from the University of Cantabria in Spain, and co-workers.
LMNA encodes Lamin proteins A and C, which are components of the nuclear envelope that protects genetic material in eukaryotic organisms.
Point mutations in this gene can have devastating consequences on the heart and skeletal muscle and, despite decades of research on lamins, no effective therapy currently exists.
In a proof-of-concept study, the team set out to develop targeted base-editing therapies for laminopathies affecting cardiac and skeletal muscle.
They selected two mutations that affect different domains of the protein that lead to distinct pathological outcomes. One, the c.T104>C (p.L35P) mutation, has been identified in patients with congenital muscular dystrophy (CMD), while the other c.G746>A (p.R249Q) mutation is linked with dilated cardiomyopathy with conduction defects.
The team developed two distinct approaches capable of targeting different mutation types to show that LMNA-associated cardiac disease could be corrected using base editing. This included an adenine base editing (ABE) approach that enabled a nucleotide conversion from adenine to guanine (A-to-G) to correct the R249Q mutation and a cytosine base editing (CBE) strategy that enabled the conversion of cytosine to thymine (C-to-T) for the L35P variant.
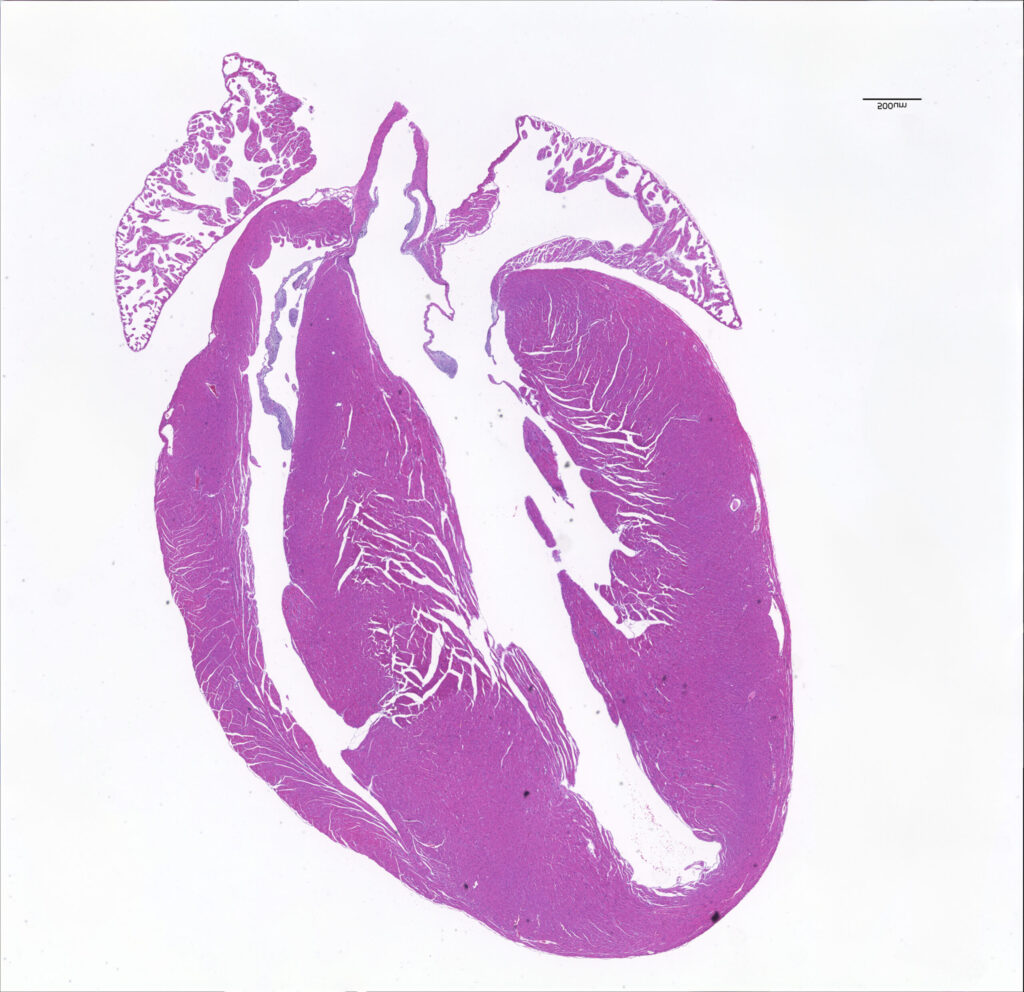
Caravia and colleagues demonstrated the efficacy of these techniques using patient-derived cardiomyocytes and mouse models carrying the human LMNA mutations.
Induced pluripotent stem cell–derived cardiomyocytes (iPSC-CMs) harboring either the L35P or the R249Q mutation showed nuclear alterations, increased DNA damage, and abnormal contraction and calcium ion transients.
The team then modeled these pathogenic conditions in vivo among “humanized” mouse models carrying the human mutations that create the disease.
Homozygous R249Q mice developed severe cardiac conduction abnormalities, cardiac arrhythmias, and died prematurely while homozygous L35P mice displayed pronounced muscle wasting and a shortened lifespan. Additionally, heterozygous L35P mice developed dilated cardiomyopathy.
Precise correction of the mutations in iPSC-CMs successfully rescued all in vitro abnormalities.
In addition, delivery of the base-editing components using an adeno-associated virus prevented pathological phenotypes and extended the lifespan of mice carrying the LMNA L35P and the R249Q mutations.
Among the base-editing strategies, ABE achieved 25% on-target editing at the level of complementary DNA and importantly less than five percent of nonsynonymous bystander editing was detected. For CBE, this increased to nearly 40%, with no non-synonymous bystander editing detected.
“Remarkably, we did not detect any off-target editing at the top eight predicted sites in any of our strategies,” the authors reported.
“All these findings demonstrate that both BE strategies are efficient and specific and that it is not necessary to correct all [cardiomyocytes] to achieve significant structural and functional benefit.”