You’ve all seen the videos—the heart-melting, tear-jerking ones where a deaf child is sitting in a doctor’s office as their cochlear implant is turned on for the first time. Almost immediately, their eyes light up, parents start crying—you start crying. Lawrence R. Lustig, MD, professor and chairman of otolaryngology, head, and neck surgery at Columbia University Medical Center and New York Presbyterian Hospital, has witnessed this remarkable experience many times.
That isn’t what happens with the deaf children who received DB-OTO, a gene therapy developed by Regeneron that aims to treat profound congenital deafness caused by mutations in the otoferlin (OTOF) gene. Lustig didn’t see an immediate reaction. In fact, he didn’t see anything.
But days and weeks later, he started getting videos from treated children’s parents. “I’ve got videos the parents sent me, saying, ‘they can hear me now,’” Lustig told Inside Precision Medicine. “The kids are running around the house screaming all of a sudden and listening to their own voices.”
The gradual improvement in hearing with DB-OTO doesn’t mean that the gene therapy isn’t effective; it’s indicative of DB-OTO working in a way that cochlear implants never could—by naturally healing the inner-hair cells critical for hearing. In a study published in the New England Journal of Medicine, Lustig and colleagues reported early results from the phase I/II CHORD clinical trial (NCT05788536). In 12 children with OTOF-related deafness who received DB-OTO, nine had hearing improvements, six could register soft speech, and three had gene therapy that normalized hearing sensitivity.
“It’s beyond our imagination how well this treatment is working,” said Lustig. “In my clinical practice, I have treated both adults and children with hearing-related disorders for nearly 30 years. Traditionally we would use cochlear implants to treat these kids. Gene therapy has been discussed in our field for years, and now we’re finally doing it. Not only are we implementing gene therapy, but it is also effective; in some cases, it shows significant success. We’re taking kids who would have otherwise been cochlear implant candidates and giving them a molecular solution so they can hear naturally. It’s one of the most exciting times in my career and my colleagues are just witnessing it.”
Mic check
Before the genomic era, audiologists like Jonathon Whitton, AuD, PhD, could measure what a child couldn’t hear but not why. “During my time in the clinic, we often saw children with congenital deafness,” Whitton told Inside Precision Medicine. “We could diagnose severity, but usually we didn’t understand why they had hearing loss. We could inform the family that we had completed the tests, that their child could not hear these sounds, and that we would develop a management plan. But we were never able to explain exactly why their child had hearing loss.”
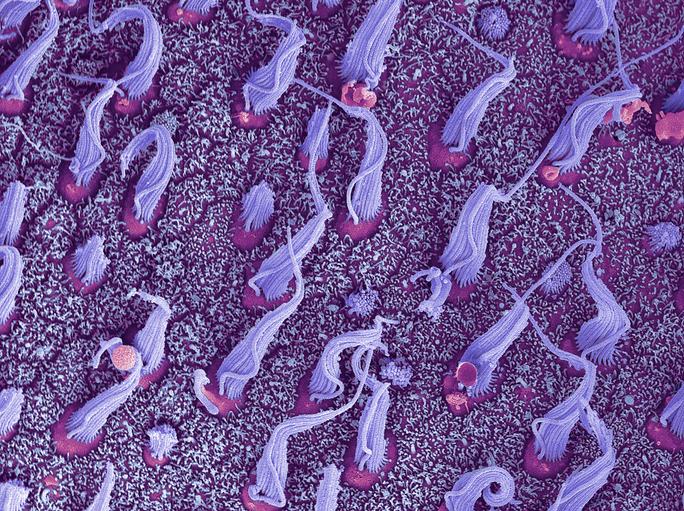
The inner ear, with its delicate hair cells and sensory neurons, has long been a black box because there are no good methods to look in the ear, Whitton said. “We don’t really have [imaging methods] yet for the ear. The diagnosis was ‘geographic,’ an issue with the sensory structures in the ears, but we cannot determine the specifics beyond that.”
That began to change as genetic testing became more common. “When we began genetic testing on many of these kids, we found that more than half of them had a genetic cause of hearing loss,” Whitton said. “And then we started to realize, hey, there’s this whole group of kids. They have profound loss of hearing. It looks like they’re missing this one single protein.”
That protein is otoferlin, encoded by the OTOF gene, a critical calcium sensor for transmitting sound signals from the ear’s inner hair cells to the auditory nerve. When the otoferlin protein is absent, the ear’s sensory structures can detect sound, but they can’t send the electrical signals onward—like a microphone with a wire that doesn’t work. Also, the amplifier—in this case, the brain—is unaffected.
That insight created an opening—a window for gene therapy. Whitton, who is now vice president and global program head for auditory therapies at Regeneron, said, “We believe there may be a period when gene addition therapy could significantly improve hearing in these children, potentially transforming their condition from complete deafness to very good hearing.”
“There are over 150 genes that can lead to hearing loss,” Lustig explained. “This one is interesting because the OTOF gene affects only one critical part of the auditory system—the inner hair cells that send sound to the brain. The outer hair cells, which feed sound back from the brain to regulate that incoming signal, are still intact. So you’ve got a situation where the hardware is all there, but the connection’s broken. The gene therapy basically restores that connection.”
Because of this unique biology, many infants with OTOF-related deafness initially pass standard newborn hearing screens. “You screen newborns with a technique called otoacoustic emissions, which measures the outer hair cells. Those work fine in these kids,” Lustig said. “But they still can’t hear. That’s why we strongly encourage using auditory brainstem responses (ABRs) for newborn screening—otherwise many will be missed until much later.”
Ear to the grindstone
Around 2008 or 2009, Lustig’s lab had an important discovery showing how to restore hearing in some animal models of genetic deafness. That launched Lustig on a whole pathway of cochlear gene therapy, and by 2019, Lustig’s team had successfully restored normal hearing in animals with OTOF-related deafness.
Shortly after Lustig had begun working on genetically restoring hearing in mice, Regeneron launched the DB-OTO program nearly nine years ago—a time when few believed in gene therapy. The company’s research team, led by Whitton and collaborators like Lustig, faced daunting challenges. Chief among them: the OTOF gene is too large to fit inside a single adeno-associated virus (AAV), the most common vehicle for gene delivery.
“When we first started on the program, we were excited about working on it from a biological perspective,” said Whitton. “But we were worried from a technological perspective because we said, hey, this gene is too big to fit into an AAV. We’re going to have to figure it out. We also thought we might have to develop a mini gene for this instead, which, obviously, people tried in other areas.”
Regeneron scientists explored a range of strategies, but it was Lustig and other academic collaborators who helped break through. Whitton said, “People were worried that we weren’t going to be able to get enough expression. But Larry and some others were like, let’s just try it.”
That early success became the foundation for DB-OTO’s development. “We started working with Larry during that time period,” Whitton said. “That was when we began designing the optimal vector for delivering this innovative mouse-proof concept for human use.”
Delivering gene therapy to the inner ear presents unique engineering challenges. The cochlea is small, enclosed, and exquisitely sensitive to disruption. “We figured out pretty early that because we’re delivering a high concentration of the vector into a relatively small space—and we’re delivering it right next to the target tissue—we seemed to overcome a lot of the inefficiencies that people face with the dual-vector approaches,” Whitton explained.
The next hurdle was ensuring precise control of protein expression. “We found that the biggest challenge was making sure we expressed the protein very specifically,” Whitton said. “So optimizing the molecule became our main focus before taking it into the clinic. Larry played a big part in that.”
A minor study with major implications
The CHORD study began dosing patients roughly three years ago and is already showing promise strong enough to support regulatory filings before the end of this year, according to Whitton. “This trial is a registrational trial,” Whitton said. “We predefined our endpoints, that’s what you can see in the manuscript, and we intend to start regulatory filings for this program before the end of the year. We’re moving very fast on this program because we think that there’s a lot of urgency there for treating these patients, and we think the data are quite compelling.”
For families, the impact is profound. As Lustig described, seeing a child turn at the sound of their mother’s voice—without an implant, without external hardware—is an emotional experience unlike anything in medicine. “To me, the most impactful thing as I’ve been going through the program has been hearing what the parents are saying,” Whitton said. “The data have been really remarkable, and it’s been incredible to see these responses on all of the clinical assessments. But the big impact has been hearing from the families.”
Lustig shared an anecdote of another child that was dosed with DB-OTO that has stuck with him. “You can see the brain re-learning how to process sound, which is extraordinary,” said Lustig. “At first she was scared with this sensation coming. She didn’t know what to make of it. She completely freaked out in the audiometric booth when we were testing her hearing. Now she’s totally excited. She loves to get her hearing checked. Her mom just sent me a video last week of her walking behind her, calling the kid’s name, and the kid turned around and smiled at her.”
The results have impressed both regulators and clinicians. For the first time, a one-time gene addition therapy appears capable of restoring natural hearing—not electronic approximation, but real sound perception. “Now there are five efforts worldwide actually using a similar technique to do gene therapy in kids with OTOF-related hearing loss.”
The auditory program has also set a new model for how industry, academia, and families can collaborate in translational science. “We’ve had a fantastic experience working with clinical sites, families, and leaders in the field like Larry,” Whitton said. “They’re incredibly excited to see this development reach patients in their lifetime after a long journey for many.”
While this rare genetic form of deafness affects only about 30 to 50 children per year in the U.S, the implications extend beyond hearing. The knowledge gained from DB-OTO—how to deliver large genes and how to accurately target specific sensory cells—could benefit other medical fields where fragile, hard-to-reach tissues have slowed down advancements.
So, while the approach may not be a blockbuster drug and lacks the instant cinematic payoff of a cochlear implant switch-on, the quiet miracle of a child turning at the sound of their name—for the first time in their life—is something deeper. It’s not just hearing restored. It’s establishing a connection never heard before.