A study published today in Cell has revealed the existence of “craters” on the surface of melanoma tumors that seem to be essential for immune cells to successfully infiltrate and kill the cancer cells. Results point out the possibility that these physical regions may provide a valuable biomarker to predict which patients will respond to checkpoint inhibitor immunotherapy.
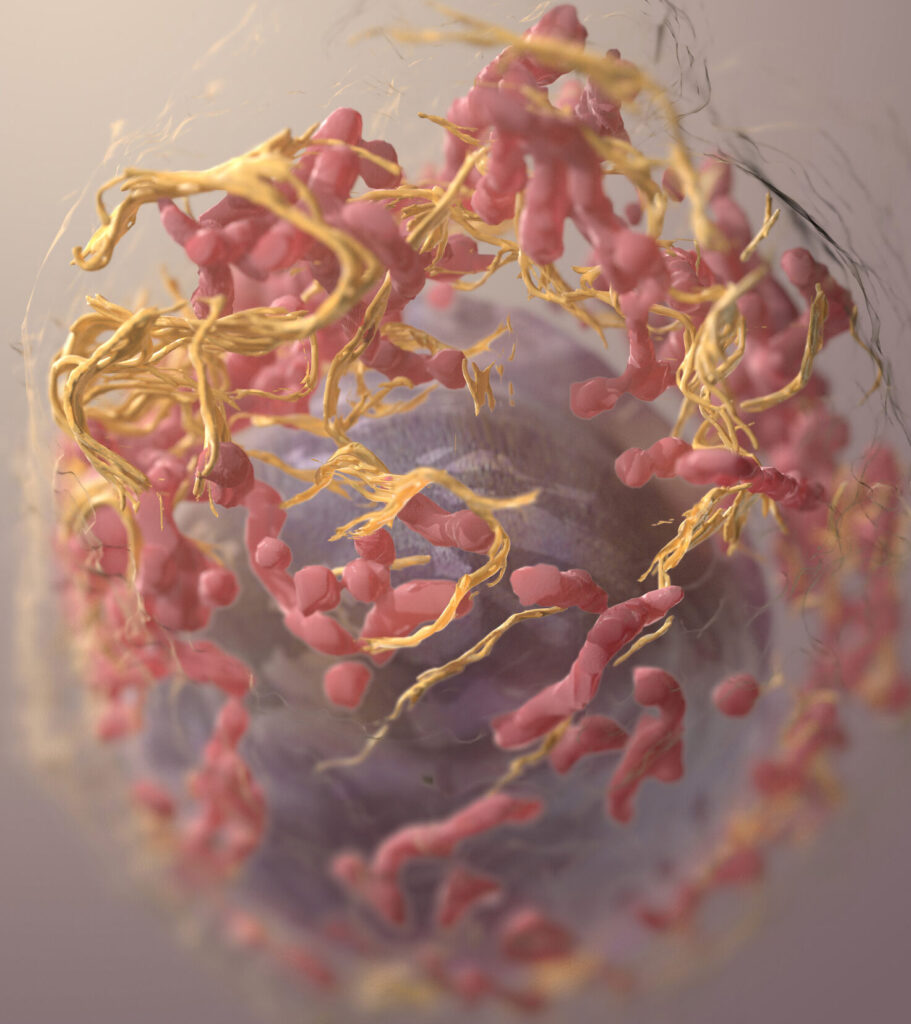
“We found that rather than patrolling the entire tumor surface, CD8+ T cells aggregated in pockets on the melanoma border, forming prolonged interactions with melanoma cells,” says Leonard Zon, MD, director of the stem cell program at Boston Children’s Hospital and senior author of the study. “We termed these pockets Cancer Regions of Antigen presentation and T cell Engagement and Retention (CRATERs) and saw that, following immune stimulation, the CRATERs expanded and facilitated an effective immune response against the tumor.”
Predicting whether a patient will benefit from immune checkpoint inhibitors remains a major challenge. While there are markers available to indicate the levels of T cell infiltration and activation within tumors, there is still limited knowledge about what enables infiltrated T cells to kill cancer cells and shrink the tumor.
To better understand the dynamic interactions between T cells and melanoma tumors, Zon and colleagues initially studied this process in zebrafish, which make imaging much easier due to being transparent. Due to common genetic features of melanoma among these fish and humans, introducing a cancer-driving mutation in the BRAF gene allowed the research team to follow the interactions between T cells and melanoma tumors in real time, for periods of up to 24 hours.
Combining this imaging technique with high-resolution spatial transcriptomics, the scientists were able to identify key regions located right in the boundary between the tumor and their surrounding environment. These CRATERs were found to be rich in antigen recognition molecules, and they harbored the highest density of killer T cells within the tumor. Furthermore, when stimulating the immune response in the zebrafish, these regions expanded in size while the number of active tumor-killing T cells in the area increased.
These CRATERs were also found in humans with a melanoma diagnosis. Among these patients, an increase in the density of CRATERs found in biopsies taken before and after receiving immune checkpoint inhibitors was linked with a positive clinical response to the treatment. Similar clusters were also found in patients with non-small cell lung cancer (NSCLC), hinting at the possibility of CRATERs being a common feature of a successful immune response across solid tumors rather than just being a phenomenon unique to melanoma.
Based on these findings, the researchers propose that measuring CRATER density could be useful as an early biomarker and diagnostic indicator to help determine the efficacy of immune checkpoint inhibitor therapy. The researchers are now planning a clinical trial to validate the use of CRATERs as a biomarker for the success of checkpoint inhibitor immunotherapy. “Pending thorough clinical verification and taken together with other measurements, CRATERs may serve to more accurately assess the efficacy of an ongoing treatment and improve treatment outcomes,” said Zon.